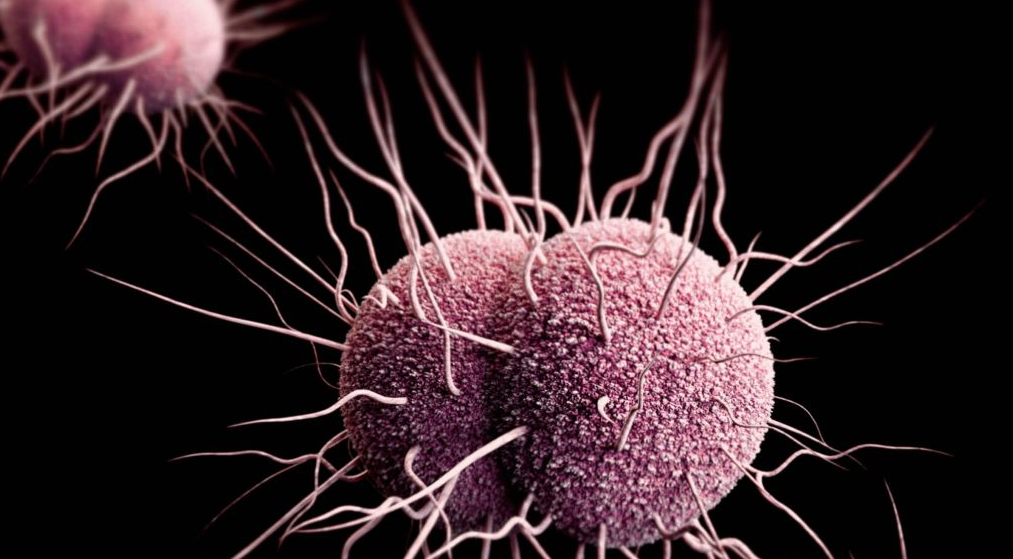
STDs : Drug-Resistant Gonorrhea, How to Fight It Off
Imagine a world where gonorrhea treatment is no longer effective. Doctors in the UK recently reported a case of drug-resistant gonorrhea that didn’t respond to what’s called “dual therapy” – giving the patient the prescribed doses of azithromycin and ceftriaxone, two of the medications most commonly used in the US and recommended by the CDC. The patient eventually was cured, but only after giving him a much higher dose, which also has its own implications on the patient.
The good news is that CDC monitors how fast gonorrhea is becoming resistant, and we have not yet seen any ”super bugs” that can’t be treated here the US. But it is highly likely that drug-resistant gonorrhea is in our future.
More than 350,000 people are diagnosed with gonorrhea in the US each year. That’s just what’s reported: the CDC estimates that more than 800,000 new infections may actually occur each year. The rate of infections among gay men increased 20% between 2009 and 2013. The rate of resistance is also increasing: the levels of resistance of gonorrhea to azithromycin increased more than 300% between 2013 and 2014. It is evolving at a faster rate than drug companies are finding new drugs to treat it. As recently as 2006, CDC had five recommended treatment options. In the US, we now are down to one.
We are not in crisis mode, so don’t hit the panic button yet. Still, we should be in “prepare” mode, which could mean better use of prevention tools. Gonorrhea resistance to new drugs builds and grows. However, there aren’t many alternative drugs in the pipeline right now for gonorrhea. This will take some time, but in the meanwhile, it’s best to get tested every three months so you can get treated if you need it.
Important, little-known fact about testing: it is not enough to pee in a cup. Gonorrhea can also infect your throat and your rectum. In fact, most gonorrhea in gay men is missed if you just do urine testing. It’s possible to have your urine test show no evidence of being infected with gonorrhea, even though you can still have an infection in your throat or rectum. Ask your doctor about getting your throat and rectum swabbed for gonorrhea and chlamydia testing. Most people have no symptoms so the only way to know is to get tested.
If you don’t want to talk to your primary care doctor about your sex life, there are other places to get tested. There are plenty of clinics that can test and treat you in a confidential and competent way. The CDC has a directory that is searchable by zip code at https://gettested.cdc.gov/.
For more information about drug-resistant gonorrhea, go to: http://www.cdc.gov/std/gonorrhea/arg/.
We’d like to hear from you: what has made it easy to ask your doctor about your sexual health needs?
Stephen Hicks
National Coalition of STD Directors



Since prep has become more prevelant in our community my sex life has gone down the tubes because I know people in our community are being less safe as if HIV is the only thing we need to worry about. Boys pay attention this is why we still need to be safe. Sadly now I only except handjobs from strangers anything else needs to be safe or I don’t play.
and in a few months we’ll get another prep article and all the barebackers will come and complain about being stigmatized
So true.